Orthopaedics 360 INFO
Shoulder bursitis is a common issue, causing difficulties with overhead movements and pain. It can come out of the blue, or due to irritation from repetitive movements. When it is suspected, there are a number of things that can be done before considering surgery. A shoulder bursa is a normal part of the shoulder, and acts to reduce friction between the bone and the rotator cuff. The underlying reason for bursitis is important, or it can return after treatment is completed.
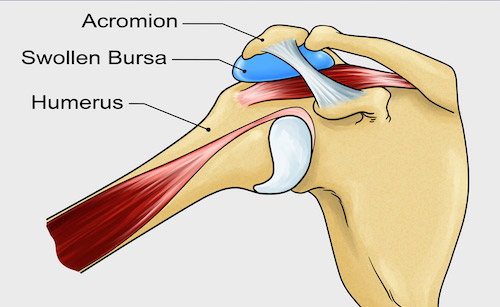
The image on the left shows the subacromial bursa. This is one of the most common forms of bursitis and can cause a lot of troublesome symptoms, including:
- Difficulties with all overhead activities
- Inability to lie on your side
- Night pain
- Inability to reach behind your back
- Pain radiating to the neck
Once shoulder bursitis is suspected, non operative management is the mainstay of treatment.
Shoulder subacromial bursitis is usually best treated with non operative management during the first few months. often, the pain can be reduced considerably, and function can be improved. Often an operation is not required. The following is a list of things that should be attempted before contemplating surgery.
- Physiotherapy is very important is reducing the symptoms of subacromial bursitis. When the bursa is inflamed, the small muscles (rotator cuff muscles) of the shoulder are deactivated, and this worsens the condition. The rotator cuff muscles act to hold the ball and socket in the correct alignment, which reduces pressure on the bursa. Physiotherapy can, on its own, reduce the symptoms of bursitis.
- Anti-inflammatory medication – Taken in short spurts, this can be a safe and effective method to reduce pain. Anti-inflammatory medication can interact with other medications, so ensure that you check with your doctor first. You should only take this sort of medication on a short burst regimen. A few days on and then a few days off
- Steroid injections into the shoulder are useful, and can be performed with or without ultrasound guidance. Local anaesthetic and steroid are injected into the bursa, causing the burial inflammation to decrease. An injection on its own will not cure bursitis as physiotherapy is required to maintain the effects of the injection, if it is to be long lasting.
- Avoidance of overhead and aggravating activities.
Operative Treatment
Once non operative management has been attempted, some people will not recover. Some patients have a bursa that is too enlarged, inflamed and thickened for the modalities above to work. When a bursa has been inflamed for a very long time, it may be harder for non operative management to be successful. Once the decision to perform a subacromial decompression is contemplated, then an ultrasound and Xray can show whether there is anything else associated with the bursitis, such as a rotator cuff tear, or a bone spur. Subacromial decompressions can be performed using an open or key-hole (arthroscopic) technique. Dr Liew uses the arthroscopic technique for all subacromial decompressions.
A subacromial decompression is performed using key hole surgery, a special device to remove the bursa, and then a motorised burr to remove any bone spurs. There are no movement restrictions post operatively.
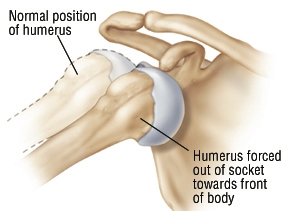
Shoulder Dislocation
Orthopaedics 360 INFO "A Place to Learn" A shoulder dislocation can occur with sporting activities, or an accident where the arm is forced into an awkward position. The most common type of dislocation is called an "anterior" dislocation, where the ball (humeral head)...
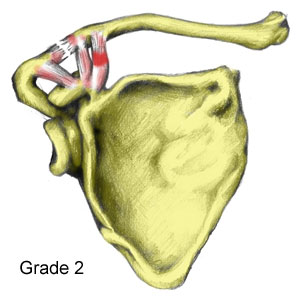
Acromioclavicular Joint Dislocation
We are currently creating fantastic new content to help our patients navigate the world of Arthritis and Sports Injury management. Please check back shortly Orthopaedics 360 INFO "A Place to Learn" An Acromioclavicular (AC) Joint disruption is fairly common, and...
Shoulder Arthritis
Shoulder arthritis limits range of motion and function. LEARN MORE
Orthopaedics 360
Orthopaedics 360
P: (08) 7099 0188
F: (08) 7099 0171
Southern Specialist Centre
Orthopaedics 360
P: (08) 7099 0188
F: (08) 7099 0171
Health @ Hindmarsh
Orthopaedics 360
P: (08) 7099 0188
F: (08) 7099 0171